Your gut is more than just a digestive system—it’s a complex ecosystem that influences everything from your immune function to your mental health. With trillions of microorganisms working in harmony, your gut microbiome plays a crucial role in your overall wellbeing. Recent scientific breakthroughs have revealed just how deeply connected gut health is to numerous aspects of human health, sparking what many experts now call “The Gut Health Revolution.”
Understanding Your Gut Microbiome: The Foundation of Digestive Wellness
The human gut contains trillions of microorganisms that form a complex ecosystem
The term “gut microbiome” refers to the vast community of microorganisms living in your intestines. Each person has approximately 200 different species of bacteria, viruses, and fungi in their digestive tract. While some microbes can be harmful, many are incredibly beneficial and necessary for optimal health.
Your gut microbiome begins developing at birth and continues to evolve throughout your life. Factors like delivery method (vaginal vs. cesarean), breastfeeding, diet, environment, and medication use all influence its composition. This microscopic world affects your body in remarkable ways:
Nutrient Processing
Gut bacteria help break down complex carbohydrates and dietary fibers that your body can’t digest on its own. They produce short-chain fatty acids and synthesize essential vitamins like B12 and K.
Immune Function
Up to 80% of your immune cells reside in your gut. The microbiome trains your immune system to distinguish between helpful and harmful microbes, preventing both infections and autoimmune reactions.
Brain Connection
The gut-brain axis allows bidirectional communication between your digestive system and brain. Certain bacteria produce neurotransmitters like serotonin that influence mood, cognition, and mental health.
Research has found connections between gut health and numerous conditions, including inflammatory bowel disease, diabetes, obesity, cardiovascular disease, autoimmune disorders, and even mental health conditions like anxiety and depression.
The Power of Fiber: Your Gut’s Most Important Nutrient

Fiber-rich foods provide essential nourishment for beneficial gut bacteria
Dietary fiber is perhaps the most crucial element for maintaining a healthy gut microbiome. Unlike other nutrients, fiber isn’t primarily for you it’s food for your gut bacteria. When these beneficial microbes digest fiber, they produce short-chain fatty acids that nourish your gut lining and reduce inflammation.
Types of Fiber That Support Gut Health
| Fiber Type | Food Sources | Benefits for Gut Health |
| Soluble Fiber | Oats, barley, legumes, apples, citrus fruits | Slows digestion, feeds beneficial bacteria, produces short-chain fatty acids |
| Insoluble Fiber | Whole grains, nuts, seeds, vegetable skins | Adds bulk to stool, promotes regular bowel movements, prevents constipation |
| Resistant Starch | Green bananas, cooled potatoes, rice, legumes | Acts as a prebiotic, reduces inflammation, improves insulin sensitivity |
| Prebiotics | Garlic, onions, leeks, asparagus, chicory root | Selectively feed beneficial bacteria, enhance microbial diversity |
Most Americans consume only 10-15 grams of fiber daily—far below the recommended 25-30 grams for women and 30-38 grams for men. This fiber gap contributes to poor gut health and associated conditions like constipation, bloating, and inflammation.
Trending Gut Health Practices: Beyond Fiber

While fiber forms the foundation of gut health, several other practices have gained popularity for their potential to enhance digestive wellness. These approaches complement a fiber-rich diet and can further support your gut microbiome:
Probiotics: Living Microorganisms for Gut Balance
Probiotics are live beneficial bacteria similar to those naturally found in your gut. Research suggests they may help restore microbial balance, particularly after antibiotic use or during digestive disturbances.
Probiotic Food Sources:
- Yogurt with live active cultures
- Kefir (fermented milk drink)
- Sauerkraut (fermented cabbage)
- Kimchi (Korean fermented vegetables)
- Miso (fermented soybean paste)
- Kombucha (fermented tea)

Fermented Foods: Traditional Wisdom for Modern Guts
Fermentation is an ancient preservation technique that creates environments where beneficial bacteria can thrive. These foods deliver both probiotics and unique compounds that support digestive health.
Did you know? A 2021 Stanford study found that a diet high in fermented foods increased microbial diversity and reduced inflammatory markers more effectively than even a high-fiber diet.
Hydration: The Overlooked Gut Health Essential

Proper hydration is crucial for digestive function. Water helps break down food, absorb nutrients, and maintain the mucus lining of your intestines. Research shows that people who drink more water have lower levels of harmful bacteria associated with gastrointestinal infections.
Aim for at least 8 glasses (64 ounces) of water daily. Herbal teas and water-rich foods like cucumbers, celery, and watermelon also contribute to your hydration status.
Actionable Tips for Improving Your Gut Health

Transforming your gut health doesn’t happen overnight, but consistent small changes can lead to significant improvements. Here’s a practical roadmap to better digestive wellness:
1. Gradually Increase Fiber Intake
Adding too much fiber too quickly can cause gas, bloating, and discomfort. Instead, gradually increase your intake by 5 grams per week until you reach the recommended 25-38 grams daily.
Sample Fiber-Rich Day Plan:
- Breakfast: Oatmeal (4g) with berries (3g) and chia seeds (5g)
- Snack: Apple (4g) with almond butter (3g)
- Lunch: Lentil soup (8g) with whole grain bread (3g)
- Snack: Hummus (3g) with vegetable sticks (2g)
- Dinner: Quinoa bowl (5g) with roasted vegetables (4g)

2. Diversify Your Diet
Different gut bacteria thrive on different foods. Aim to eat 30+ different plant foods weekly, including a variety of:
Vegetables
Leafy greens, cruciferous vegetables, root vegetables, and colorful varieties provide different fibers and phytonutrients.
Fruits
Berries, apples, citrus, and tropical fruits offer varying types of fiber, antioxidants, and polyphenols that feed beneficial bacteria.
Whole Grains
Oats, quinoa, brown rice, barley, and ancient grains like farro and amaranth provide resistant starches and different fiber types.
3. Incorporate Fermented Foods Daily
Try to include at least one serving of fermented foods in your daily routine. Start with small amounts (1-2 tablespoons) and gradually increase to avoid digestive discomfort.
4. Manage Stress Levels

The gut-brain connection means stress directly impacts digestive function. Chronic stress can alter gut bacteria composition and increase intestinal permeability (“leaky gut”). Implement stress-reduction techniques like:
- Meditation or mindfulness practice (10-15 minutes daily)
- Regular physical activity (30+ minutes most days)
- Adequate sleep (7-9 hours nightly)
- Deep breathing exercises
- Time in nature
5. Limit Gut-Disrupting Foods and Substances
Foods That Support Gut Health
- Fiber-rich whole foods
- Fermented foods
- Polyphenol-rich foods (berries, dark chocolate, green tea)
- Omega-3 rich foods (fatty fish, walnuts, flaxseeds)
- Prebiotic foods (garlic, onions, leeks, asparagus)
Foods That May Disrupt Gut Health
- Ultra-processed foods with additives and emulsifiers
- High-sugar foods and beverages
- Excessive alcohol consumption
- Artificial sweeteners
- Refined carbohydrates
Addressing Common Digestive Issues
Even with a focus on gut health, many people experience digestive discomfort. Understanding these common issues can help you address them effectively:

Bloating and Gas
Occasional bloating affects most people, but chronic bloating may indicate an underlying issue. Common causes include:
- Rapid eating (swallowing excess air)
- Certain FODMAP foods (fermentable carbohydrates)
- Sudden increase in fiber intake
- Food intolerances
- Imbalanced gut bacteria
Evidence-based solution: Try a food journal to identify trigger foods. Eat slowly, chew thoroughly, and consider digestive enzymes with meals. For persistent bloating, consult a healthcare provider to rule out conditions like SIBO (small intestinal bacterial overgrowth).
Irritable Bowel Syndrome (IBS)
IBS affects 10-15% of the global population and involves symptoms like abdominal pain, altered bowel habits, bloating, and gas. While the exact cause remains unclear, gut-brain interactions, altered gut microbiota, and food sensitivities play significant roles.
“The gut microbiome in IBS patients typically shows reduced diversity and altered composition compared to healthy individuals. Targeted dietary interventions can significantly improve symptoms in many cases.”
Evidence-based approaches for managing IBS include:
- Low-FODMAP diet (under professional guidance)
- Gut-directed hypnotherapy
- Stress management techniques
- Regular physical activity
- Specific probiotic strains

Constipation
Infrequent bowel movements (fewer than three per week) or difficult passage of stool affects many people. Beyond discomfort, chronic constipation can disrupt gut microbiota balance.
Evidence-based solutions include:
- Gradually increasing fiber intake to 25-30g daily
- Staying properly hydrated (minimum 64oz water daily)
- Regular physical activity
- Establishing a consistent bathroom routine
- Considering magnesium supplementation (consult healthcare provider)
When to see a doctor: Consult a healthcare provider if you experience persistent changes in bowel habits, blood in stool, unexplained weight loss, severe abdominal pain, or if symptoms don’t improve with lifestyle modifications.
The Gut-Brain Axis: How Your Digestive System Affects Your Mind
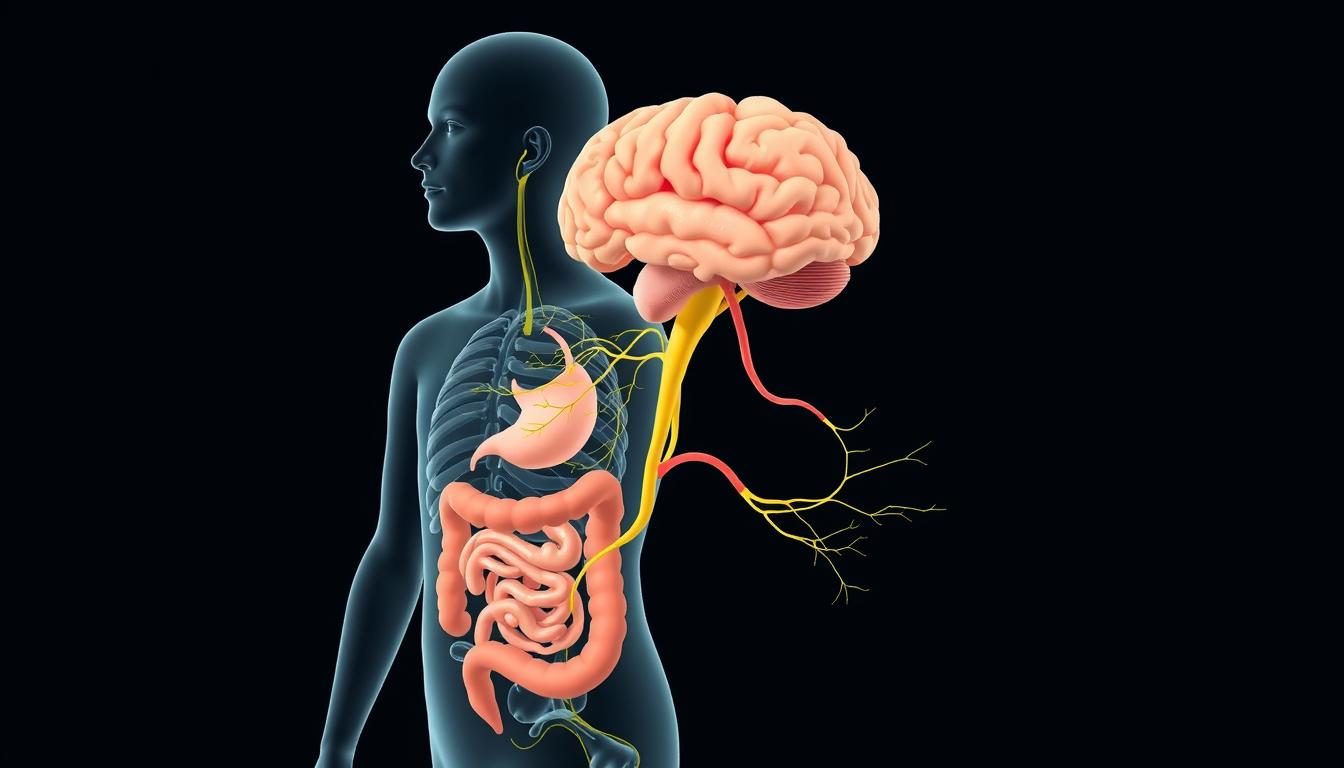
One of the most fascinating aspects of gut health research is the discovery of the gut-brain axis—a bidirectional communication network between your digestive system and brain. This connection explains why digestive issues often coincide with mental health challenges and vice versa.
How Your Gut Communicates With Your Brain
Your gut and brain communicate through multiple pathways:
- Vagus nerve: The primary neural connection between gut and brain
- Neurotransmitters: Gut bacteria produce serotonin, GABA, and dopamine
- Immune signaling: Inflammatory molecules can affect brain function
- Microbial metabolites: Bacterial byproducts influence brain activity
Research has found connections between gut health and conditions like anxiety, depression, autism spectrum disorders, and even neurodegenerative diseases like Parkinson’s and Alzheimer’s.
“The gut microbiome produces hundreds of neurochemicals that the brain uses for the regulation of basic physiological processes, including learning, memory and mood. In fact, 95% of the body’s serotonin is produced by gut bacteria.”
This emerging field suggests that supporting gut health may be a complementary approach to managing certain mental health conditions, though more research is needed before specific clinical recommendations can be made.
Frequently Asked Questions About Gut Health
How quickly can I expect to see improvements in my gut health?
Some changes, like reduced bloating from eliminating trigger foods, may be noticeable within days. However, meaningful shifts in gut microbiome composition typically take 2-4 weeks of consistent dietary and lifestyle changes. More significant improvements in conditions like IBS may take 2-3 months of dedicated effort.
Are probiotic supplements necessary for good gut health?
Not necessarily. While specific probiotic strains may benefit certain conditions, most people can support their gut microbiome through diet alone. Fermented foods, fiber-rich plants, and diverse whole foods often provide better results than supplements. If you do choose a probiotic, look for one with multiple strains and at least 1 billion CFUs (colony-forming units).
Can antibiotics permanently damage gut health?
Antibiotics can significantly disrupt gut microbiota, with effects lasting weeks to months. However, most healthy microbiomes can recover with proper support. If you need antibiotics, consider taking them with food (unless contraindicated), finishing the full course as prescribed, and focusing on prebiotic and fermented foods afterward to support recovery.
How does gut health affect weight management?
Research shows that gut microbiome composition differs between individuals with obesity and those of healthy weight. Certain bacteria may influence how we extract and store energy from food, affect appetite regulation, and impact insulin sensitivity. While improving gut health alone isn’t a weight loss solution, it may support metabolic health and complement other weight management strategies.
Is leaky gut syndrome real, and should I be concerned?
Increased intestinal permeability (“leaky gut”) is a real physiological phenomenon where the intestinal barrier becomes more porous, potentially allowing bacterial products and food particles to enter the bloodstream. While some alternative health practitioners attribute numerous conditions to leaky gut, the scientific community is still researching its exact role in disease. Focusing on general gut health principles—fiber, whole foods, stress management—supports gut barrier function regardless.

Embracing the Gut Health Revolution
The science is clear: your gut microbiome plays a crucial role in your overall health and wellbeing. By prioritizing fiber-rich foods, incorporating fermented options, staying hydrated, managing stress, and limiting gut-disrupting substances, you can cultivate a thriving internal ecosystem that supports both physical and mental health.
Remember that gut health is highly individualized – what works for someone else may not work for you. Pay attention to how your body responds to different foods and practices, and be patient with the process. Sustainable improvements come from consistent, moderate changes rather than extreme approaches.

As research continues to uncover the far-reaching impacts of gut health, one thing becomes increasingly evident: the foods we eat and the lifestyle choices we make profoundly influence our microbiome, which in turn affects virtually every aspect of our health. By embracing the principles outlined in this article, you’re not just improving digestive comfort—you’re investing in your long-term health and vitality.
Get well and keep well,
Ray.


